The WPSC Speak-Up! Award
Next nomination deadline is January 31, 2026
You may submit at any time. Nominations submitted beginning June 1 will automatically go toward the December 31st award.
Did you know that seeing a problem and speaking up about it before it does harm is a strong indicator of a positive organizational culture of safety?
The Washington Patient Safety Coalition (WPSC) Speak-Up! Award is a statewide recognition program to celebrate staff and teams who voice their concerns to keep patients and staff safe, and their organizations that create work environments to encourage them to do so.
When someone or a team is nominated for this award they did the right thing for patients and staff and their actions serve as a model to others.
The WPSC Speak-Up! Award is open to individuals and teams from any Washington healthcare organization from hospitals to pharmacies.
If you are interested in how speaking up and awards like this can make a difference please read Adam Novak’s article “Improving safety through speaking up: An ethical and financial imperative.” in the Journal of Health Care Risk Management, Vol 39, No. 1.
We want to thank the Michigan Health & Hospital Association Keystone Center PSO and the Virginia Hospital and Healthcare Association for their support. This program is modeled after similar awards in Michigan, Virginia, and Minnesota.
Award Deadlines
– January 31, 2026
– June 30, 2026
You may submit at any time. Nominations submitted after an award period closes will automatically go toward the next award period.
Nomination Information
Here’s a TIP:
Use your organization’s good catch program as a source for nominations.
- The description of the event is very important.
- Events that lead to shared learning and changes in processes, policy, procedures, etc., are highly valued.
- Nominations are submitted via the Nomination Form button on this page. It’s fast and easy.
- Please omit any Protected Health Information.
- Nominations should be for events within the past 12 months.
- This is an award for clinical and non-clinical team members. Nominations are for submitted by a person from a healthcare organization on behalf of the person or people who made a good catch or spoke up. They may be staff or a patient/resident/family member or a combination of all.
- The WPSC Speak-Up! Award is open to individuals and teams from any Washington healthcare organization, such as hospitals, pharmacies, long term care (e.g. skilled nursing facilities & assisted living facilities), clinics and physician offices to name some examples.
- You can nominate the same individual or team multiple times, but it must be for different events.
- There is a limit of one award finalist per facility, per award cycle. All organizations and staff are still encouraged to nominate as many individuals as they would like, however, only one nominee will move into the finalist pool per award cycle.
- Application and supplementary materials provided during the nomination process will not be returned.
- Please check submissions for completion and eligibility. Any submissions with issues are replied to as not accepted with an explanation.
Below are examples of completed nomination forms. They include all questions in the form.
Its important to use the last question, which is a short description of the event, to elaborate on your responses to the other questions. For example: Why wouldn’t somebody else have caught this? Why would someone remain silent? What barriers to speaking up exist in the organization? What changes did the organization make?
Example 1
| Organization Name | General Hospital |
| Organization Address | 705 2nd, Seattle, WA 98101 |
| Nominator Name | Stan Smith |
| Nominator Organizational Email | ssmith@gh.org |
| Nominator Title/Position | MHA RNBN, PSO |
| Nominator Phone | 206-555-1212 |
| Nominee Name(s) | Sarah Wright |
| Nominee Organizational Email(s) | swright24@gh.org |
| Nominee Phone | 206-555-1212 X113 |
| Nominee Title/Position(s) | RN, Oncology |
| What type of adverse event or error was prevented? i.e. medication error, fall, etc. | Medication Error; Inappropriate Treatment |
| Did a patient, family member, or advocate speak up or initiate the “good catch”? | No |
| If the nominee(s) hadn’t spoken up, what is the likelihood that this could have ended as a “near miss”? | Unlikely |
| If the nominee(s) hadn’t spoken up, do you think that somebody else may have caught this? | Unlikely |
| If the nominee(s) hadn’t spoken up, what is the likelihood that the patient/resident/staff would have incurred permanent damage? | Likely |
| If the nominee(s) hadn’t spoken up, what is the likelihood that the patient/resident/staff could have died? | I’m Not Sure |
| Was the decision to speak up spontaneous or premeditated? | Spontaneous |
| Would it have been easy to have remained silent? | No |
| Did the nominee(s) encounter barriers to speaking up (such as somebody brushing off their concern)? | No |
| Was the patient, resident, family or representative informed of the concern? | Yes |
| Did the organization make any changes as a result of speaking up? | No |
| Please include as much anecdotal information below that you are comfortable disclosing about the event (please omit protected health information): |
This event involves a situation where an order was placed for Irradiated Packed Red Blood Cells (PRBCs) for an oncology patient, but what arrived at the bedside were non-irradiated PRBCs. Through investigation, it was found that a number of “Swiss-cheese holes” led to the wrong blood product arriving at bedside. Thanks to the RNs commitment to patient safety, her actions prevented an immunocompromised patient receiving a product that could have put them at risk for a rare but serious complication (transfusion-relatedgraft-versus-host disease). The RN identified that the PRBCs were not irradiated, through paying attention to detail (STAR: Stop Think Act Review). She spoke up for safety by contacting transfusion services to raise concern about the blood product delivered (CUS: Concern; Uncomfortable; Stop). The patient and family was informed of the of the event and an apology was issued as well as how the organization will investigate and make changes to the process. The end result of the RN speaking up was a new order process that was implemented throughout the health system. |
Example 2
| Organization Name | Infusion Specialists, Inc. |
| Organization Address | 705 2nd, Seattle, WA 98101 |
| Nominator Name | Lisa Lu |
| Nominator Organizational Email | llu22@isi.org |
| Nominator Title/Position | Safety and quality analyst |
| Nominator Phone | 206-555-1212 |
| Nominee Name(s) | Infusion Team |
| Nominee Organizational Email(s) | fmarks@isi.org |
| Nominee Phone | 206-555-1215 |
| Nominee Title/Position(s) | Team Lead, RN PCA PAA HUC |
| What type of adverse event or error was prevented? i.e. medication error, fall, etc. | Medication order, dosing, administration, treatment error |
| Did a patient, family member, or advocate speak up or initiate the “good catch”? | No |
| If the nominee(s) hadn’t spoken up, what is the likelihood that this could have ended as a “near miss”? | Very Likely |
| If the nominee(s) hadn’t spoken up, do you think that somebody else may have caught this? | No |
| If the nominee(s) hadn’t spoken up, what is the likelihood that the patient/resident/staff would have incurred permanent damage? | Very Likely |
| If the nominee(s) hadn’t spoken up, what is the likelihood that the patient/resident/staff could have died? | Very Likely |
| Was the decision to speak up spontaneous or premeditated? | Spontaneous |
| Would it have been easy to have remained silent? | Yes |
| Did the nominee(s) encounter barriers to speaking up (such as somebody brushing off their concern)? | Yes |
| Was the patient, resident, family or representative informed of the concern? | Yes |
| Did the organization make any changes as a result of speaking up? | Yes |
| Please include as much anecdotal information below that you are comfortable disclosing about the event (please omit protected health information): |
I would like to respectfully nominate the Infusion Team for The Washington Patient Safety Coalition (WPSC) Speak-Up! Award. The Infusion team cares and administers treatments for patients who need outpatient intravenous therapies such as chemotherapies, immunotherapies, blood transfusions, IV fluids, antibiotics, and a lot of other specialty medications via intravenous, subcutaneous, or intramuscular routes. Staff cares for 80-90 patients daily in this fast-paced, complex department. From the front desk staff, patient care assistants, nurses, and leadership, all members of the Infusion Team go above and beyond the care of patients every day. There have been several near misses that saved a patient’s life because of the whole teams’ dedication and commitment to patient safety and patient care. 1. Medication order error. 2. Medication dosing error. 3. Advocating for Patient Safety 4. Advocating for Patient Safety These few examples and many others are testament to the Infusion Teams’ daily show of dedication, pride, and commitment to patient care and patient safety. This Team embodies excellent teamwork and accountability, especially in challenging situations. The strength of this team is not just in individual members. The strength of each member IS the team! Together, they make a difference by speaking up and preventing patient harm. |
Evaluation Process
All nominations will be reviewed by WPSC staff and a committee of patient safety and quality improvement leaders and patient advocates. All nominations are deidentified before going to the committee.
- The first step is for WPSC staff to evaluate the completeness of the nomination form, the nature of the event and the impact of the prevented adverse event or error. There are a total of 33 points, out of 103, in step 1. If a nomination advances to step 2, the nominator may be asked to provide additional information.
- Each nomination advancing to step 2 is considered a finalist and will receive a notification email and recognition.
- In the second step, the committee will judge each finalist using the following criteria in addition to evaluating applications and supplemental nomination materials for a total of 70 points out of 103.
- Severity of the prevented adverse event
- Magnitude of the decision to speak-up
- Level of difficulty of speaking-up
- Effect of speaking-up on the organization
- Based on the total points accumulated the committee will select the Speak-Up! Award winner(s). Yes, the committee has the discretion to award more than 1 winner per award period.
Award Presentation
- All award recipients will be notified individually.
- All nominees are congratulated and receive recognition through the WPSC’s website and patient safety newsletter. Finalists and award winners will receive recognition at the annual NW Patient Safety Conference. Award recipients will receive free registration to the conference. If approved by the awardee’s organization, the WPSC will arrange for an onsite recognition event.
- The WPSC may publish the nominee’s name if selected as a finalist. Please email WPSC@qualityhealth.org if you would not like your name shared.
Award Winners
May 31, 2025
Award Recipients
Annie Pham, RN and Nicole Spencer, RN, Harborview Medical Center. Annie and Nicole identified that a patient had not been appropriately monitored due to discontinued lab orders. This resulted in better integration of lab and infusion orders across all UW Medicine hospitals.

Finalists:
- Awet Negash, RN, Kindred Hospital Seattle, Empowered by ScionHealth
- Katra Noor, CNA, Kindred Hospital Seattle, Empowered by ScionHealth
- Kailey Bolles, MD, Harborview Medical Center
- Rebecca Beal, RN, MultiCare HealthCare System, Capital Medical Center
- Clifton Jones, Facilities Management Department, MultiCare Healthcare System, Tacoma General Hospital
- Jens Moren, Facilities Management Department, MultiCare Healthcare System, Tacoma General Hospital
December 31, 2024
Award Recipients
Rona Dujon, RN, Psychiatry Geriatric, MultiCare Auburn Medical Center. Rona identified mislabeled crash carts, which spurred a system-wide correction to enhance patient safety.

Finalists:
- Minchi McCartin, Pharmacist, Kindred Hospital Seattle, Empowered by ScionHealth
- Barb St. Onge, Pharmacist, Kindred Hospital Seattle, Empowered by ScionHealth
- Jeff Greagrey, MRI Technician, MultiCare Covington Medical Center
- Brent Kirhsenbaum, Pharmacist, MultiCare Auburn Medical Center
- Janette Connolly, Emergency Service Technician, MultiCare Auburn Medical Center
May 31, 2024
Award Recipients
Ryan Boyd, MRI Technician at Multicare Healthcare System- Covington. Ryan’s insistence on stopping an imaging procedure prevented a patient from incurring permanent harm.
Bethelhem Semere, RN at Kindred Hospital Seattle Empowered by ScionHealth. Bethelhem’s attention to detail and persistence prevented a very serious event due to the unidentified incomplete removal of a Nasogastric tube.

Finalists:
- Jenny Phillips, Respiratory Therapist, Multicare Healthcare System – Valley Hospital
- Katie Mertens, Surgical Technologist, UW Medicine – Valley Medical Center
- Michael Peden, Respiratory Therapist, MultiCare HealthCare System – Tacoma General Hospital
- Rae Gordon, Core Lab Technician Assistant, Multicare Healthcare System – Good Samaritan Hospital
- Shana Thach, Nutrition Assistant, MultiCare HealthCare System – Tacoma General Hospital
December 2, 2023
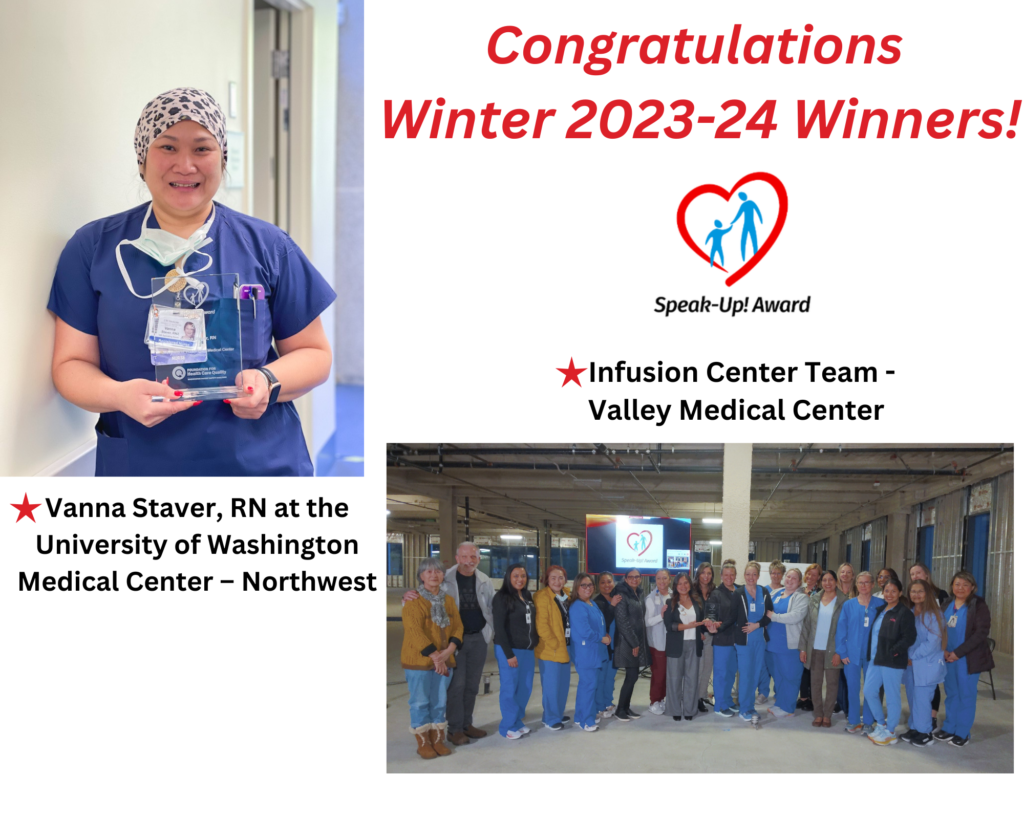
Award Recipients
Individual award: Vanna Staver, RN at the University of Washington Medical Center – Northwest prevented what could have been permanent harm from a wrong site surgery. Speaking up for safety, especially in the operating room where authority gradient can be apparent, takes courage and is supported by the Northwest’s psychologically safe work culture. Because of Vanna’s speaking up for safety, the organization has identified opportunities related to surgical site marking standards and implemented quality improvement changes to ensure the process is reliable and safe, every time.
Team award: Infusion Center Team, Valley Medical Center – Stopping The Line when there is a patient concern, re-assessment of the situation, speaking up, and intervening to prevent patient harm prevented medication errors. From the front desk staff, patient care assistants, nurses, and leadership, all members of the Infusion Team embody excellent teamwork and accountability, especially in challenging situations. Speaking up resulted in greater collaboration with ordering providers leading to improved trust between providers and nurses.
Finalists
- Michelle Bunikis, OR Staff Nurse – University of Washington Medical Center
- Holy Ige, RT; Zeek Lebbie, CAN; Adam Alhassan, Security – Kindred Hospital Seattle, Empowered by ScionHealth
- Meaza Woldemichael, Nurse – Kindred Hospital Seattle, Empowered by ScionHealth
- Suhair Hamza, Nurse – Kindred Hospital Seattle, Empowered by ScionHealth
- Nicholas Anderson – University of Washington Medical Center
May 31, 2023 Award
Award Recipient
Dani Morton, OB Surgical Technologist, University of Washington Medical Center, for preventing an unintentional retained foreign object through professional persistence.
Finalists
- Rajani M. Ward, Gynecological Oncology RN, Swedish Cancer Institute
- Miranda Todd, RN, Harborview Medical Center
- Joshua Gothberg, Pharmacy Tech A, Multicare Healthcare System
- Scott VanHorn, Pharmacist Supervisor, NorthStar Lodge, Multicare Yakima Valley Memorial Hospital
December 2, 2022 Award
Award Recipient
- Julia Ganey, Clinical Staff Pharmacist, Providence Swedish Cherry Hill Campus, for speaking up to identify areas of improvement in the identification and treatment of heparin induced thrombocytopenia (HIT) that resulted in multi-disciplinary education and changes in workflow.

Finalists
- Jennifer Legg, Inpatient Pharmacy Manager & Inpatient Pharmacists, Providence Swedish Edmonds Medical Center
- Lynne Freeman, Family Medicine, Valley Medical Center
- Karol Draeger, Admitting Registrar, Valley Medical Center
- Shannon Gaskin and Freddy Ruiz, Molecular FISH laboratory technicians, CellNetix Pathology and Laboratories
July 8, 2022 Award
Award Recipients
- Nursing Team on 8EH – Burns, Plastics & Pediatric Trauma Acute Care Unit at Harborview Medical Center (HMC), for continuing their commitment to ensure integration of medical interpreters in clinical activities.
- ICU/Tele Team, Swedish Issaquah Medical Center, for preventing potential overdoses due to drug ingestion involving patients in possession of illegal substances and outside medications.

Finalists
- Barbara Brenneman, Pharmacist, Swedish Medical Services
- Hannah Baldwin, Occupational Therapist, Swedish Health Services
- Ian Geiger, RN and Young Mi Murphy, RN, Ambulatory Surgery, Swedish Health Services
- ICU/Tele Team, (RNs/NACs/MTs/HUCs), Swedish Issaquah Medical Center
- Jolene Silzell, Grossing technician, CellNetix Laboratories and Pathology
- Katy Brehe, RN2- Trama Surgical ICU, Harborview Medical Center
- Nursing Team on 8EH – Burns, Plastics & Pediatric Trauma Acute Care Unit, Harborview Medical Center
- Roz Parsons, Nurse Manager, Valley Medical Center
- Sajar Camara, PET CT Technologist, Swedish Health Services
Frequently Asked Questions
Who can be nominated?
The WPSC Speak-Up! Award is open to clinical and non-clinical staff. Nominees may be individuals or teams from any Washington healthcare organization, such as hospitals, pharmacies, long term care (e.g. skilled nursing facilities & assisted living facilities), clinics and physician offices to name some examples. This award is founded on the principle of transdisciplinary teamwork; everyone has the right to be concerned and everyone has the right to speak up.
Can I nominate myself?
Yes, you may nominate yourself, though we will require another contact at your facility to verify the authenticity of the event.
Are submissions protected from disclosure?
Yes. The WPSC is a Federally listed Patient Safety Organization. Submissions are considered Patient Safety Work Product and protected under the Patient Safety & Quality Improvement Act.
•Not subject to subpoena in civil, criminal, administrative proceedings
•Not subject to discovery
•Not admissible into evidence
•Not subject to Freedom of Information Act
•Data cannot be disclosed except as permitted under the Act/regulations
Can patients, residents and families be nominated?
Not at this time. This award is focused on acknowledging the efforts of healthcare staff. However, the roles of patients, residents and families should be acknowledged if part of the narrative.
How many times can I nominate an individual or team?
You can nominate the same individual or team multiple times, but it must be for a different event. If two nominations are submitted for the same event, we will reach out to the contacts listed in the nomination forms to work with each nominator.
Is there a limit on the number of nominees from each organization?
There will be a limit of one award finalist per organization, per period. All organizations and staff are still encouraged to nominate as many individuals as they would like, though only one nominee will move into the finalist pool per period.
Can a nominee receive this award even if information about the event is withheld?
Yes, though we do encourage you to submit as much information as possible, we realize that certain information is sensitive.
How old can the good catch or event described in the nomination be?
Nominations are for events no older than 12 months.
Will any of our information be published?
We would like to share your Speak-Up! story in a de-identified manner if possible, but will always respect the wishes of you and your organization. None of the details of the event within your nomination form will be published unless otherwise approved by both you and your organization.


