The 19th Northwest Patient Safety Conference
“Advancing Patient Safety in Today’s World”
October 18th and 19th, 2022
Presented in collaboration with the Oregon Patient Safety Commission and the BC Patient Safety and Quality Council
For those that were able to attend the live conference, we hope you enjoyed it!
The conference sessions are recorded!
Recorded Presentations:
The conference presentations will be posted on the conference event portal on November 7. To view the recorded presentations, log into the event portal here and enter your attendee confirmation code (you can find your attendee confirmation code at the very bottom of your registration confirmation email, if you can’t obtain it, please contact Amelina Kassa at akassa@qualityhealth.org.) Once you are logged into the portal, click on the “General Info” tab at the top of the page. The presentations, slides, and supporting materials will all be posted there sorted by presentation date and time.
 C.E. Credit Information:
C.E. Credit Information:
HOW TO APPLY FOR CE CREDITS FOR THE LIVE CONFERENCE PRESENTATIONS:
All conference registrants should have received an email with subject “SURVEY/C.E. APPLICATION: 2022 NW Patient Safety Conference” sent by email wpsc@qualityhealth.org. If you were registered and did not receive the survey email, please contact Amelina Kassa at akassa@qualityhealth.org so you can get the link emailed to you and take the survey. For CE credits go directly to question 12. However, we encourage you to complete the entire survey and provide us with feedback! Upon receipt of your survey/CE application, we will either send you a certificate(s) or for Nursing Contact Hours we will send you a required questionnaire about each presentation.
HOW TO APPLY FOR CE CREDITS IF YOU VIEW THE RECORDED PRESENTATIONS:
CE CREDITS FOR ALL PRESENTATIONS ARE NO LONGER AVAILABLE
In the event portal, toward the top of the “General Info” page is a section called “How to get educational credits.” In this section is a link to a CE application form used for the recordings. Use this for all recorded presentations. Upon receipt of your CE application, we will send you the certificate(s).
The Conference Committee
Dana Kahn – Chair Jamie Leviton
Amelina Kassa Jeff Goldenberg
Andrea Wnuk Jonathan Stewart
Anita Sulaiman Karen Brigham
David Birnbaum Naomi Kirtner
Havaei Farinaz Rex Johnson
Jackie Valentine Valerie Harmon
Keynote Presentations
Click on the Speakers tab to the left for the full list of presenters
Jessie Singer, author of: “There Are No Accidents.” Going beyond the traditional system approaches we’re used to hearing about, Jessie brings a fresh and expanded perspective to harm reduction. You’ll view safety systems not only as tangible mechanisms, but as social systems. Jessie is a journalist whose writing appears in The Washington Post, The Atlantic, The Nation, Bloomberg News, BuzzFeed, New York magazine, The Guardian, and elsewhere.
Anne Roberts and panel of advocates: “Lessons Learned from “Dr. Death”.
We invite you to hear the story of the now infamous case of Christopher Duntsch, aka “Dr. Death”, firsthand, from the physicians that petitioned the Texas Medical Board to revoke Dr. Duntsch’s license, and the attorneys that they partnered with to prosecute him in criminal court resulting in his current life sentence in prison. This case highlighted significant failures in the healthcare system that contributed to the death and/or permanent injury of 33/38 patients that he operated on.
Michelle Schreiber, MD, Deputy Director, Center for Clinical Standards and Quality, Centers for Medicare and Medicaid Services: The 2022 CMS Quality Strategy, CMS Levers of Safety. Dr. Schreiber will discuss the CMS National Quality Strategy that focuses on a person-centric approach from birth to death as individuals journey across the continuum of care. While past CMS strategies attained important achievements, in many cases they have not been sustained or been inclusive of underserved communities. On April 12, 2022, the agency launched the CMS National Quality Strategy, an ambitious long-term initiative that aims to promote the highest quality outcomes and safest care for all individuals.
Carole L. Hemmelgarn and Martin Hatlie: “Who killed patient safety?” Carole, Marty, Susan Sheridan and Beth Daley Ullem wrote the provocative opinion piece “Who killed patient safety?” in the May 5th edition of the Journal of Patient Safety and Risk Management. If you haven’t read it, do. While the World Health Organization and its member states are ramping up efforts, it appears to us that patient safety is adrift in the United States. The organizations who used to oversee, lead, and support safety have moved on to other priorities. Safety is no longer a critical part of their strategies, oversight, and programmatic funding. It is time those organizations and others do a deeper pause on their work to contemplate if they are leading in safety or they are complicit in the decline of safety in the U.S. She will discuss why patient safety has fallen off the national agenda and identify how patients’ advocates can be the catalyst to revitalizing patient safety.
Armando Nahum, Patients for Patient Safety: Engaging Patients and Families in Quality and Safety: A deep, transparent partnership. In 2006, Armando Nahum and his wife Victoria began their work in patient advocacy and engagement by establishing Safe Care Campaign after 3 members of his family became infected in 3 different hospitals, in 3 different states in 10 months’ time, culminating with the death of his son, Josh. He was 27. He will describe the importance of Patient Experience and the Key Benefits of Person and Family Engagement. We’ll take a peek at the next generation of Patient and Family Advisory Councils and will describe the current state of Patient and Family Advisory Councils due to the pandemic and our current solution to rejuvenate them.
In addition to the keynotes there are seven breakout sessions with regional, national and international experts, thought leaders and your colleagues’ sharing tools and experiences on such topics as: restorative approaches after healthcare harm, tools to improve diagnosis, responding to culture of safety surveys, alternatives to traditional informed consent, burnout and wellness, shared decision making, impact of technology, “patient ergonomics”.
Registration is closed.
 Total presentations: 12
Total presentations: 12
Fees:
- Healthcare professionals and anyone seeking continuing educational credits, $75
- Patients, their families, and students, Free
- Discounts are offered for registrants with CPPS, CPHQ and BCPA certifications.
Payments accepted: all major credit cards via PayPal.
Continuing educational credits for the 2022 conference are no longer available
*Recorded educational credit availability is determined by the accrediting organization. See table below for credits. Attendees will request CE credits via a conference survey following the conference or via a form on the recorded conference website. PLEASE NOTE THE CREDIT AMOUNTS MAY CHANGE IF THE AGENDA CHANGES.
| Credit Type | Total Credits for Live Conference | Credits Available for Recordings |
| BCPA | 2.5 ethics 10.5 general Click here for Approved Program Content (live & recorded) |
Yes – up to the 2.5 ethics Live up to the 10.5 general Live |
| Nursing Contact Hours |
13.8 Approved by the California Board of Registered Nursing, Provider Number CEP 16359 for 13.8 contact hours |
Yes – total sessions viewed must exceed 60 minutes to receive credit |
| CPHQ | 12.67 | Yes, up to the 12.67 Live |
| CPPS | 12.5 Click here for Approved Program Content (live and recorded) |
Yes, up to the 12.5 Live |
Questions? Contact wpsc@qualityhealth.org or call Steve Levy, Executive Director, 206-204-7383.
Anne Roberts and Panel - Lessons Learned from “Dr. Death”
The now infamous case of Christopher Duntsch, aka “Dr. Death”, has highlighted significant failures in the healthcare system that contributed to the death and/or permanent injury of 33/38 patients that he operated on. The physicians that petitioned the Texas Medical Board to revoke Dr. Duntsch’s license, and the attorneys that they partnered with to prosecute him in criminal court resulting in his current life sentence in prison, invite you to hear their story, firsthand.
The panel will discuss the following:
• The complications discovered post-operatively for some of the most egregious of Duntsch’s cases
• The failure to disclose pertinent information from the training program, ensure sufficient training and significant conflicts of interest
• The failure of several hospital’s peer review programs and the Texas Medical Board to properly address significant complaints/peer review issues in a timely manner
• The breakdown at hospitals that inappropriately granted temporary privileges, ignored credentialing red flags or placed profit over patient safety
• How it took the criminal justice system, not the healthcare/peer review system, to ultimately stop him
• What physician leaders and administrators can do to strengthen their credentialing & peer review processes to avoid these pitfalls
Learning Objectives:
• How the case went from malpractice to criminal
• System Failures that contributed to the injury of 33/38 patients he operated on
• Lessons learned and tips to avoid this type of failure within the overall healthcare system
Armando Nahum, Patients for Patient Safety - Engaging Patients and Families in Quality and Safety: A Deep, Transparent Partnership
This session will describe the importance of Patient Experience and the Key Benefits of Person and Family Engagement. We’ll take a peek at the next generation of Patient and Family Advisory Councils and will describe the current state of Patient and Family Advisory Councils due to the pandemic and our current solution to rejuvenate them.
Learning objectives:
• Connecting the head with the heart
• Redefine Person and Family Engagement
• The importance of the Patient’s voice to improve Safety
Carole Hemmelgarn and Martin Hatlie - Who Killed Patient Safety?
Carole, Martin Hatlie, Susan Sheridan and Beth Daley Ullem wrote the provocative opinion piece “Who killed patient safety?” in the May 5th edition of the Journal of Patient Safety and Risk Management. If you haven’t read it, do. While the World Health Organization and its member states are ramping up efforts, it appears to us that patient safety is adrift in the United States. The organizations who used to oversee, lead, and support safety have moved on to other priorities. Safety is no longer a critical part of their strategies, oversight, and programmatic funding. It is time those organizations and others do a deeper pause on their work to contemplate if they are leading in safety or they are complicit in the decline of safety in the U.S. She will discuss why patient safety has fallen off the national agenda and identify how patients’ advocates can be the catalyst to revitalizing patient safety.
Learning objectives:
• Discuss why patient safety has fallen off the national agenda.
• Identify how patients advocates can be the catalyst to revitalizing patient safety.
Session pre-work
You may wish to read the short opinion piece “Who killed patient safety?” from the May 5th edition of the Journal of Patient Safety and Risk Management.
Chris Goeschel (New Tools for Improving Diagnosis) - Improving Diagnostic Capacity: It takes a Team, Tools, and Tenacity
This session will provide a succinct overview of Diagnostic Improvement Tools and resources developed under a multiyear contract from the Agency for HealthCare Research and Quality. (Patient and Family Engagement in Diagnosis; TeamSTEPPS to Improve Diagnosis, Measure Dx; and Calibrate Dx.; along with 8 separate issue briefs on unique diagnosis related topics). PFE focuses specifically on helping patients and families speak up during the diagnostic process and understand the importance of their voice. TeamSTEPPS focuses on leveraging team contributions to diagnostic improvement; Measure Dx focuses on how organizations can identify and begin to measure opportunities for diagnostic improvement and Calibrate Dx is a tool that focuses on individual providers and the diagnostic process.
Learning objectives:
• Define diagnostic error and its’ importance as a patient safety issue
• Explain the impact of provider communication breakdowns on diagnostic safety
• Define the diagnostic team and discuss barriers to effective teamwork and how to overcome them
Haavi Morreim - Artificial Intelligence in Healthcare: Reckoning with Errors in Medical Records
Have you ever looked at your own electronic medical record (EMR)? We would like to know about your own experiences! Would you be willing to review your own medical records, as a patient and tell us about the accuracy of what you see. Log into your patient portal and review a record or two. We have a short survey for you to fill out HERE. This survey is completely anonymous – no one will know who said what. Also, this is not a scientific study. We just want to know whether you see errors in your EMR. We’ll share what we learned during this presentation.
Artificial intelligence is increasingly making its way into clinical care. On one side, it may enhance diagnostic efforts, e.g., by interpreting CT or MRI images, or pathology slides such as PAP smears. At the same time, AI in clinical decision making can carry significant hazards. Medical records (which often form the dataset for AI) appear to have far more errors than we currently recognize. Open Notes has greatly increased patients’ access to their clinical records and, in the process, revealed errors. “1 in 5 patients who read a note reported finding a mistake and 40% perceived the mistake as serious.” (Frequency and Types of Patient-Reported Errors in Electronic Health Record Ambulatory Care Notes, Sigall K. Bell, Tom Delbanco, Joann G. Elmore, et al, JAMA Netw Open. 2020;3(6):e205867). Using actual patient descriptions of errors in their medical records (through a pre-conference survey to registrants and existing data), this presentation will describe errors in medical records, share what the survey revealed, and discuss these errors’ implications for the use of Artificial Intelligence in clinical care.
Learning objectives:
- Recognize the basic definition and elements of Artificial Intelligence (AI)
- Describe current efforts toward integrating AI into clinical care, at both diagnostic and therapeutic levels
- Discuss the hazards posed by medical errors present in clinical records as an AI dataset
Jessie Singer - There Are No Accidents
“There Are No Accidents” will provide a history lesson and primer on unintentional injury death, including the current crisis, and the historical framings of injury causality. She will provide stories of the corporate profitability of an “individual blame” model and evidence of the effectiveness of a systemic harm reduction model, as well as inspiration of the effectiveness of systemic injury prevention throughout history. She will also present a new conception of the “Swiss Cheese” model that accounts for social determinants of health.
Learning objectives:
• Understanding the important differences in looking at “accident” causality through a human error vs. dangerous conditions model
• Learning why we blame human error, and why it is a disastrous tendency
• Learning what’s possible when we incorporate social determinants of health into our conception of injury prevention
Jodie Errington and Sarah Jaaskelainen - Survey Results to Tangible Actions: Maximizing Impact of the Culture of Safety Survey
This session will focus on describing an innovative approach to the development of action items that address low scoring items on Fred Hutch Cancer Center’s biennial Culture of Safety Survey (CoSS). There is a paucity of literature on how to develop and implement targeted action items to address CoSS results. The existing literature is clear that safety culture is a unit level phenomenon co-created by all disciplines that work collaboratively in that area. Our Patient Safety Team developed a triad leadership approach to ensure accountability for review, discussion, development and follow up of action items: (1) Identification of Physician, NP/PA-C and Nurse Manager triad with established accountability for their unit’s CoSS results; (2) Development of a Tableau dashboard to easily visualize clinic results and specific strengths and opportunities; (3) Patient Safety led Action Planning Meeting with triad leaders to brainstorm contributing factors for lowest scoring item and develop 1 action item targeted to address that item; (4) 3-month follow up to check-in on status of action item.
Learning objectives:
• Learn about an approach to establish multi-disciplinary creation and ownership for Culture of Safety Survey results by clinic area
• Review a practical, step by step methodology to develop an action item to target low scoring items from the Culture of Safety Survey for each clinic area
• Discuss lessons learned and specific challenges experienced throughout the development and implementation of this approach
John James - From Informed Consent to Probability Based, Shared Decision-Making
From Informed Consent to Probability Based, Shared Decision-Making John will use personal stories, legal decisions, and research findings to show how inadequate the concept of informed has become. It is being slowly replaced by shared decision-making (SDM) in which the preferences of the patient are combined with the knowledge of the clinician to optimize the patient’s medical care. He will describe ways in which SDM has fallen far short of what reasonable patients wish to know. John will describe in detail the findings of his research in which the voice of patients is finally being heard in the debate over what information should be disclosed. He will characterize the challenges of delivering SDM and how probability-based-shared decision making (PB-SDM) must replace traditional SDM to better inform patients of the risks they may be facing during their medical care.
Learning objectives:
• Learn the shortcomings of traditional informed consent
• Learn the attributes and limitations of shared decision-making
• Understand the essentials of probability-based, shared decision making
Michelle Schreiber - The 2022 CMS Quality Strategy and CMS Levers of Safety
Dr. Schreiber will discuss the CMS National Quality Strategy that focuses on a person-centric approach from birth to death as individuals journey across the continuum of care. While past CMS strategies attained important achievements, in many cases they have not been sustained or been inclusive of underserved communities. On April 12, 2022, the agency launched the CMS National Quality Strategy, an ambitious long-term initiative that aims to promote the highest quality outcomes and safest care for all individuals.
Rich Holden & Nichole Werner - Patient Ergonomics – Applying the Science of Patient Work to Design Safer Systems for Patients and Care Partners
Patient Ergonomics – the science and design of patient work – is an approach used to design safer systems by attending to the co-production work done by patients and care partners. Patient and care partner work is often unseen or underappreciated, thus these key co-producers of care are too often denied formal assistance, support, and relief from burdens and indignities. Clinicians, patients, and care partners may also make poor decisions resulting from discordant ideas about what a patient is able to do, needs, or wants. When designers fail to see patient and care partner work, they fail to design effective systems for key safety-relevant goals, such as care transitions. This presentation will describe tools and techniques from the field of patient ergonomics to study, design, and evaluate systems to support patient and care partner work.
Learning objectives:
• Apply methods for studying and designing work to the domain of patient and care partner work
• Analyze how patient work contributes to patient safety during transitions of care
• Understand consistent findings about the nature of patient work and patient work system
Robert Robson, Allison Kooijman - Restorative Practices: Enhancing Healing and Learning after Healthcare Harm
This session will briefly discuss the present structural and legislative barriers to (a) healing after healthcare harm (involving all direct participants – patients, families, communities, and healthcare providers), and (b) systemic and individual learning about a particular adverse event. The presentation will then review restorative principles and relational approaches in responding to harm events and contrast these with restorative justice. Case studies will be presented and, time permitting, a short video presentation. Finally, the presentation will review the initial experience of feasibility projects evaluating the introduction of restorative approaches after healthcare harm in two Health Authorities in B.C. will be reviewed including the course to train facilitators in restorative processes.
Learning objectives:
• Participants will understand the structural, legislative and systemic barriers to promoting learning and healing after healthcare harm
• Participants will become familiar with the principles of restorative processes and understand the nature of relational approaches
• Participants will learn about the challenges of introducing and implementing restorative approaches in healthcare.
Skye McKennon - Restorative Practices: Safe and Well: Utilizing Evidence-Based Strategies to Promote Health Professional Well-Being and Patient Safety
Healthcare professionals were exhibiting distress prior to the COVID-19 pandemic including, but not limited to, stress, emotional exhaustion, depersonalization, and burnout. The already precarious state of health professional well-being has worsened in the last several years. Research has established the correlation between health professional burnout and worsening patient safety. The need to foster well-being for the safety of both patients and professionals is urgent. This seminar will teach strategies to cultivate well-being, promote resilience, and prevent burnout in your health systems, teams, and selves. We will begin with a brief overview of burnout. This will be followed by a robust active learning session focused on evidence-based and evidence-informed tools and approaches for well-being. Interventions stemming from the systems level will be the primary focus, but team and individual strategies will also be included. The learner will leave knowing factors that contribute to burnout, the inverse relationship between resilience and burnout, proven ways to promote resiliency and well-being, and how to access useful resources.
Learning objectives:
• State the prevalence of healthcare professional burnout.
• Define moral injury.
• Outline approaches (systems-based, team-based, and individual-based) that improve healthcare professional well-being.
• Access resources to support healthcare professional well-being.

Anne Roberts and Panel - Lessons Learned from “Dr. Death”






Anne Roberts is a dual-certified and nationally recognized consultant with over 25 years of experience assisting hospitals nation-wide with developing best practice credentialing, privileging and peer review programs. She serves as Of Counsel at the award winning trial law firm of Van Wey, Metzler & Williams in Dallas, Texas representing patients and families harmed by medical errors. She is also the System Vice President, Medical Affairs Operations at Mount Sinai Health System in New York City, and an award-winning author of numerous books published with a primary focus on legal strategies to prevent negligent credentialing and privileging in healthcare systems.
The panel of advocates presenting include:
• Anne Roberts
• Martin Lazar, MD – Neurosurgeon that served as the expert reviewer for the Texas Medical Board and advocated for revocation of his license and continues to advocate for patient safety and improved credentialing & peer review processes.
• Robert Henderson, MD – Orthopedic Spine Surgeon who performed numerous corrective surgeries after Duntsch injured the patients, and advocated for the Texas Medical Board, the ACGME and the Am. Board of Neurosurgery to strengthen their programs
• Kay Van Wey – Attorney who represented a great deal of the patients harmed and worked with the prosecution to distinguish between malpractice and criminal intent
• Michelle Shugart – Dallas Assistant District Attorney who partnered with the physicians and malpractice attorneys to prosecute Dr. Duntsch for his crimes and to prevent him from being able to harm more patients
• Robert Oshel, PhD – Retired Assoc. Director for Research & Disputes at the NPDB discusses NPDB reporting requirements, common misunderstandings and statistical breakdowns of report data
Armando Nahum, Patients for Patient Safety - Engaging Patients and Families in Quality and Safety: A Deep, Transparent Partnership

Armando Nahum is the Co-Founder and President of Safe Care Campaign, an organization dedicated on Infection Prevention.
In 2006, Armando Nahum and his wife Victoria began their work in patient advocacy and engagement by establishing Safe Care Campaign after 3 members of his family became infected in 3 different hospitals, in 3 different states in 10 months’ time, culminating with the death of his son, Josh. He was 27.
The Nahums have not only turned their family’s tragedy into a positive tribute to their young son, but Armando’s educational presentations “Hospital Associated Infections: What YOU Should Know” and “Change One Thing, Change Everything” inspire hospital administrations and frontline caregivers to remind, provoke and motivate all who work in the continuum of care of their most noble challenge and moral duty to prevent these infections that annually infect more than 1.7 million and kill more than 99,000 patients in the U.S.
The story of Safe Care Campaign’s work has been featured on many national and local television and radio programs, including the CBS Evening News with Katie Couric, FOX News, CNN: The Situation Room with Wolf Blitzer and The Dr. Oz Show, as well as in numerous articles in journals and publications including Infection Control Today and CNN’s The Empowered Patient, as well as in numerous articles in journals and publications including: The Wall Street Journal, The Washington Post, The New York Times and Infection Control Today.
Armando has co-produced, with the Centers for Disease Control and Prevention (CDC), APIC and a grant from Kimberly-Clark, a patient safety video – the health care counterpart to the FAA safety demonstration that airlines are required to show passengers before every flight. The video was created to be used as part of every hospital admission to teach patients how to insist on safe care through the practice of hand hygiene.
Armando currently sits on the CDC Council on Infection Prevention, the Georgia Hospital Association Advisory Board to Prevent Infection, the Georgia Department of Public Health HAI Advisory Committee, a member of MedStar Health System Patient and Family Advisory Council for Quality and Safety (SPFACQS) and a voting member of the Presidential Advisory Council for Combating Antibiotic Resistant Bacteria (PACCARB). Along with his wife Victoria, Marty Hatlie and Dr. Tim McDonald, Armando has launched the Healthcare and Patient Partnership Institute (H2Pi) to effectively train Hospitals to achieve the stated goals of CMS’ Partnership for Patients by bringing the Patient and Family member’s voice into structured and sustainable Advisory Councils. Armando is a member of MedStar Health System Patient and Family Advisory Council for Quality and Safety (SPFACQS). He has been a driving force in establishing Patient and Family Advisory Council for Quality and Safety (PFACQS) at each of the 10 MedStar Hospitals as well as countless of PFACs across the country through a partnership with Vizient, Inc.
Carole Hemmelgarn and Martin Hatlie - Who Killed Patient Safety?


Carole Hemmelgarn, MS, MS, is the Director for the Executive Master’s program for Clinical Quality, Safety & Leadership at Georgetown University, and the Senior Director Education for the MedStar Institute for Quality & Safety. Carole graduated from Colorado State University with a degree in Speech Communication. She received a master’s degree in Patient Safety Leadership from the University of Illinois at Chicago, and a second master’s degree in Health Care Ethics from Creighton University. Hemmelgarn is involved in patient safety work across the country. She sits on the Leapfrog Patient & Family Caregiver Expert Panel, Board of Quality, Safety and Experience at Children’s Hospital Colorado, Clinical Excellence Council for Colorado Hospital Association, ABIM Foundation, Patient Advisory Committee and the Board of Directors for the Collaborative for Accountability and Improvement and Founding member of Patients for Patient Safety US.
Marty Hatlie is CEO, Project Patient Care (PPC), the Chicagoland safety and quality improvement coalition, which is dedicated to using the voice of the patient to improve care. Through PPC, he is a co-developer of the H2Pi – Healthcare & Patient Partnership Institute — suite of tools for developing Patient and Families Advisory Councils focused on improvement work. Hatlie also is President of Partnership for Patient Safety (p4ps), which produced the First Do No Harm® educational film series as a tool for advancing the reliability of healthcare systems worldwide.
Hatlie serves on the Patients for Patient Safety Advisory Group — a part of the World Health Organization’s Patient Safety Programme, as well as the Boards of Directors of the Patient Safety Movement Foundation, the Leapfrog Group, Smart Patients, Loyola MacNeal Hospital and the Alliance for Integrated Medication Management. He also has advisory roles with several bodies focused on patient safety, including the National Quality Forum’s Measure Applications Partnership Hospital Workgroup, Leapfrog Group’s Patient and Family Expert Panel, Joint Commission’s Patient Safety Advisory Group, RL Datix, and the National Action Plan to Advance Patient Safety organized by the Agency for Healthcare Quality and Research together with the Institute for Healthcare improvement.
Chris Goeschel (New Tools for Improving Diagnosis) - Improving Diagnostic Capacity: It takes a Team, Tools, and Tenacity

Dr. Christine (Chris) Goeschel is a system leader, implementation scientist and quality and safety researcher at MedStar Health. She serves as Assistant Vice President in the MedStar Institute for Quality and Safety (MIQS) and inaugural Director of the Center for Improving Healthcare Diagnosis.A professor in the Georgetown University School of Medicine, Dr Goeschel is also Associate Faculty in the Johns Hopkins Bloomberg School of Public Health, where she co-directs a required course in the Master of Hospital Administration program.
The author of over 70 peer reviewed publications, Dr Goeschel currently serves on the board of a multi hospital healthcare system in Michigan, was appointed to the National Advisory Committee for the Coalition to Improve Diagnosis, and in 2019 received a 3-year appointment from the U.S. Department of Health and Human Services to the National Advisory Council for Quality and Safety Research (NAC). Dr Goeschel is Principal Investigator for the MedStar AHRQ ACTION III contract and PI on three unique multi-year awards focused on building diagnostic capacity and improving the diagnostic process.
Haavi Morreim - Artificial Intelligence in Healthcare: Reckoning with Errors in Medical Records

Haavi Morreim, JD, PhD, is Professor, College of Medicine, University of Tennessee. She does clinical teaching, consulting, and research, with special interest in health care’s changing economics, conflict resolution, and litigation issues surrounding clinical medical research.
Dr. Morreim is also a mediator for disputes in both civil and family matters, mediating cases ranging across employment, contract, landlord-tenant, real estate and beyond. As Principal, Center for Conflict Resolution in Healthcare LLC (www.healthcare-mediation.net), she provides mediation services and training in conflict resolution for the health care setting. Dr. Morreim is a licensed attorney, assisting clients pro bono in selected cases. She has argued and won before the Tennessee Court of Appeals.
Dr. Morreim has authored two books and over 180 articles in journals of law, medicine, and bioethics. She has presented hundreds of invited lectures nationally and internationally, to such groups as the American Medical Association and the American Bar Association. Dr. Morreim is also a Fellow of the American Bar Foundation, whose membership is limited to 1% of lawyers licensed to practice in each jurisdiction.
Jessie Singer - There Are No Accidents
Jessie Singer is a journalist whose writing appears in the Washington Post, The Atlantic, The Nation, Bloomberg News, BuzzFeed, New York magazine, The Guardian, and elsewhere. She studied journalism at the Arthur L. Carter School of Journalism at New York University, and under the wing of the late investigative journalist Wayne Barrett. Her book “There Are No Accidents” is available at Simon & Schuster.
Jodie Errington and Sarah Jaaskelainen - Survey Results to Tangible Actions: Maximizing Impact of the Culture of Safety Survey


Jodie Errington is a Quality & Patient Safety Program Manager at the Fred Hutch Cancer Care (FHCC). After earning her BSN from the University of British Columbia, Jodie worked as a chemotherapy certified nurse on the inpatient oncology unit at the British Columbia (BC) Cancer Agency in Vancouver, Canada. After 8 years there, she accepted a rural-remote position with an outpatient chemotherapy unit in Northern Canada’s Yukon Territory where she was one of two oncology nurses serving the entire Territory. After spending a year and a half in the North, Jodie returned to the Pacific Northwest where she continued to work per diem at the BC Cancer Agency while providing full-time support as a Clinical Specialist with the medical technology company Becton Dickinson, Canada, specializing in vascular access and biohazard safety. Prior to her role in the Quality Department, she worked as a staff nurse and Professional Practice Coordinator on the Apheresis unit at FHCC. Jodie can be contacted at jlerring@seattlecca.org.
Sarah Jaaskelainen is passionate about innovative solutions that lead to even safer healthcare systems for those who receive and provide it. Sarah is an experienced Registered Nurse with an extensive background in Medical-Surgical, Trauma, and Emergency Nursing and has worked in Chattanooga, TN and Seattle, WA. In 2019 she earned her master’s degree in International Development / Public Health from Andrews University. Sarah currently works at Fred Hutch Cancer Center (FHCC) as a Quality and Patient Safety Program Manager. Sarah can be contacted at sjaaskelai@seattlecca.org
John James - From Informed Consent to Probability Based, Shared Decision-Making

By profession John James was a toxicologist for NASA for 25 years, having retired in 2014. He became a patient safety activist because of his son’s death due to uninformed and unethical medical care. He published a book in 2007 called A Sea of Broken Hearts – Patient Rights in a Dangerous, Profit Driven Healthcare System. He published a seminal paper in 2013 showing that medical errors cause far more deaths than the Institute of Medicine estimated. He was told that his paper was the most cited paper ever published in the Journal of Patient Safety. He testified to a Senate Subcommittee on that subject in 2014 and coedited a book called The Truth about Big Medicine in 2015. He has given patient safety talks to medical students and physicians, to law students and lawyers, to nurses and nursing students, and to the public. In 2017 He turned to making the public smarter about getting safe healthcare. In 2019 He published a seminal paper on the wishes of patients when facing an invasive procedure.
Michelle Schreiber - The 2022 CMS Quality Strategy and CMS Levers of Safety

Dr. Schreiber is currently the Deputy Director of the Center for Clinical Standards and Quality at CMS, and the Director of the Quality Measurement and Value-Based Incentives Group. While at CMS Dr. Schreiber has led many quality initiatives, including MIPS transformation to value pathways, the modernization of the Hospital Stars program, as well as advancing digital quality measurement systems. She is on the boards of ACCME (continuing medical education), Leapfrog, and a member of HITACH (the national health information advisory committee) among others. Prior to joining CMS she also participated in numerous state and national quality committees including the Board of Directors for the Michigan Hospital Association Keystone Center and the Patient Safety Organization, the Board of Directors of MPRO (Michigan Peer Review Organization – the Michigan QIO), the National Quality Forum Patient Safety Metrics Committee, and the National Quality Partners. She has worked with the Institute for Healthcare Improvement (IHI) including as part of its Leadership Alliance, the Pursuing Equity initiative, and an initiative to enhance Board of Trustees engagement in quality through a partnership with IHI and National Patient Safety Foundation. Dr. Schreiber has also served as a member of the Epic Safety Forum, and the Cerner Academic Advisory Group.
Rich Holden & Nicole Werner - Patient Ergonomics – Applying the Science of Patient Work to Design Safer Systems for Patients and Care Partners


Dr. Rich Holden is an engineer, psychologist, and academic scientist with over 20 years’ experience working to improve health and healthcare. He is an internationally recognized innovator of human-centered systems engineering tools, and his work has been published in over 150 books and articles and supported by over $75 million in federal funding. He earned a joint PhD in Industrial Engineering and Psychology from the University of Wisconsin and is now at the Indiana University School of Public Health, where he is a Professor, Dean’s Eminent Scholar, and Chair of Health & Wellness Design.
Nicole Werner, PhD is an Associate Professor in the Department of Health and Wellness Design at the Indiana University School of Public Health-Bloomington. Trained in Human Factors and Applied Cognitive Psychology, she is a systems thinker and human-centered design evangelist committed to transforming the quality and safety of healthcare for people living with chronic conditions through human-centered system design. Her research, funded by the National Institutes of Health and the Agency for Healthcare Research and Quality, has produced innovative but realistic health technology and care process interventions to improve the quality and safety of healthcare within and across healthcare settings, with a particular focus on older and vulnerable populations and their care partners.
Robert Robson and Allison Kooijman - Restorative Practices: Enhancing Healing and Learning after Healthcare Harm


Rob Robson brings more than 20 years of direct experience in the patient safety field combined with more than 30 years as a healthcare mediator and conflict engagement practitioner, to supplement his ongoing practice as a primary care physician. He obtained his Master’s in Human Factors and system Safety at Lund University in Sweden and studied under Sidney Dekker and Erik Hollnagel. Rob has participated directly and indirectly in more than 1500 adverse event reviews and has developed a systemic nonlinear approach to promote learning after such reviews.
Allison Kooijman,PhD Student, Faculty of Health and Social Development, University of British Columbia Okanagan Campus
Injured as a result of a cancer misdiagnosis, Ali speaks with firsthand experience about the harm, after harm, that results when responses to patient safety incidents are less than ideal. Ali is a former licensed practical nurse and a current PhD student at the University of British Columbia, Okanagan Campus where she explores the contributions that a restorative approach could make to changing the culture of how harm is responded to in the healthcare context. Ali is grateful to reside on the Lands of the Syilx People in Coldstream, B.C.
Skye McKennon - Restorative Practices: Safe and Well: Utilizing Evidence-Based Strategies to Promote Health Professional Well-Being and Patient Safety
Skye McKennon is an educator, pharmacist, and author with a passion to empower others to live healthier, more intentional, and more resilient lives. Dr. McKennon is the Thread Director of Pharmacology and Interprofessional Education at the Washington State University Elson S. Floyd College of Medicine, where she also serves as a Clinical Associate Professor. She is a licensed pharmacist and board-certified pharmacotherapy specialist with over a decade of experience as a faculty member. She has experience delivering well-being, burnout prevention, and resiliency workshops and continuing education sessions for healthcare professionals regionally and nationally and has authored multiple book chapters and textbooks related to pharmacy, integrative health, and mind/body medicine.

We are pleased to invite interested sponsors to support our 19th annual conference. As a sponsor you are helping to subsidize the cost of the conference to healthcare staff and provide free attendance to patients, families, and students.
THIS YEAR’S PACKAGES OFFER SEVERAL LEVELS FROM WHICH TO CHOOSE.
Details of package benefits are described in the application.
- Platinum Sponsor – $10,000 (1 available)

- Gold Sponsor(s) – $7,500 (3 available)
- Silver Sponsor(s) – $5,000
- Bronze Sponsor(s) – $2,500
- Supporter(s) of Patient Safety – $1,500
All sponsors will be recognized on the Washington Patient Safety Coalition website and marketing materials with sponsor logos linking to a webpage of your choice.
Platinum, Gold, Silver and Bronze sponsors have access to a dedicated page on the conference website which can include images, videos, links, etc.

The Polyclinic and The Everett Clinic joined Optum in 2019. Optum is a nationwide family of doctors dedicated to connecting every aspect of health and health care and making it simpler. Together, we’re making health care work better for everyone.
Our partnership with Optum means we’re able to expand our services and locations to offer even more services. As we grow, we’ll keep on delivering top-quality care to the community, just as we always have.
One of our goals is to serve more patients. And that means we’ll keep on working with and accepting a wide range of health plans.
It also means The Polyclinic and The Everett Clinic are working together across the Puget Sound to offer personalized health care, close to where residents live and work. As always, we’re here to offer the care and support patients need to live their healthiest lives.
Please visit HERE for more information!
DAY 1 – Tuesday, October 18, 2022 8:00 A.M. - 1:00 P.M. (PST)

DAY 2 – Wednesday, October 19, 2022 8:00 A.M. - 12:30 P.M. (PST)

Continuing educational credits: Attendees are eligible for Nursing Contact Hours, CPHQ, CPPS and BCPA educational credits. These may be acquired by attending the live sessions or watching the recorded sessions through October 31, 2023. *Recorded educational credit availability is determined by the accrediting organization. See table below for credits. Attendees will request CE credits via conference survey following conference or via form on recorded conference website.
| Credit Type | Total Credits for Live Conference | Credits Available for Recordings |
| BCPA | 2.5 ethics 10.5 general (Approved Program Content (live & recorded) |
Yes – up to the 2.5 ethics Live up to the 11.5 general Live |
| Nursing Contact Hours | 13.8 Approved by the California Board of Registered Nursing, Provider Number CEP 16359 for 13.8 contact hours |
Yes – total sessions viewed must exceed 60 minutes to receive credit |
| CPHQ | 12.67 | Yes, up to the 12.67 Live |
| CPPS | 12.5 | Yes, up to the 12.5 Live |
CE questions? Contact wpsc@qualityhealth.org or call Steve Levy, Executive Director, 206-204-7383.

For those that were able to attend the live conference, we hope you enjoyed it and learned plenty!
If you were not able to attend the live conference, not to worry, we will be uploading the conference sessions in the event portal on November 7. To gain access to the portal and watch the sessions, you will be required to enter your attendee confirmation code that you can find at the bottom of your registration confirmation email. If you have any trouble getting in, please contact Steve Levy at 206-204-7383 or Amelina Kassa at 206-204-8384.
C.E. Credit Information:
HOW TO APPLY FOR CE CREDITS FOR THE LIVE CONFERENCE PRESENTATIONS:
All conference registrants should have received an email with subject “SURVEY/C.E. APPLICATION: 2022 NW Patient Safety Conference” sent by email wpsc@qualityhealth.org. If you were registered and did not receive the survey email, please contact Amelina Kassa at akassa@qualityhealth.org so you can get the link emailed to you and take the survey. For CE credits go directly to question 12. However, we encourage you to complete the entire survey and provide us with feedback! Upon receipt of your survey/CE application, we will either send you a certificate(s) or for CNEs we will send you a required questionnaire about each presentation.
RECORDED PRESENTATIONS:
The conference presentations will be posted on the conference event portal on November 7. To view the recorded presentations, log into the event portal at the “enter event portal here” button above and enter your attendee confirmation code (you can find your attendee confirmation code at the very bottom of your registration confirmation email, if you can’t obtain it, please contact Amelina Kassa at akassa@qualityhealth.org.) Once you are logged into the portal, click on the “General Info” tab at the top of the page. The presentations, slides, and supporting materials will all be posted here sorted by presentation date and time.
HOW TO APPLY FOR CE CREDITS IF YOU VIEW THE RECORDED PRESENTATIONS:
In the event portal, toward the top of the “General Info” page is a section called “How to get educational credits.” In this section is a link to a CE application form used for the recordings. Use this for all recorded presentations. Upon receipt of your CE application, we will send you the certificate(s).

ART SPEAKS
For the second year, WPSC’s Addressing Stigma & Bias Workgroup is featuring artwork as a powerful way to connect with patients’ experiences with health conditions. Our focus this year is mental illness & behavioral health.
Art is not only beautiful, it is a potent medium of expression. Evocative and compelling, it touches the soul and connects in a way no other medium can.
Featured artwork this year include art and a poem by PNW residents Louie Gong, Mahvish Naqvi, Munira Leslie Sinclair and Anita Sulaiman as well as a poem by model-turned actress and mental health advocate, Cara Delevingne. Big thank you to the artists for sharing their compelling pieces with us.
**************************************************************************************************************************************************************************
Visual Art
**************************************************************************************************************************************************************************

ART PIECE: Black Sheep
Click here for a video showing the making of this piece
ARTIST NAME: Louie Gong
Click here for artist’s biography and link to Eighth Generation.
ARTIST INFO: Louie Gong (Nooksack) is the founder of Eighth Generation. A self-taught artist who was raised by his grandparents in the Nooksack tribal community in northwest Washington, he got his start by painting cultural art on shoes.
Realizing that creating one-of-a-kind pieces did not provide a sustainable pathway to success, he began applying his artwork to accessibly priced products. His unique style merges traditional Coast Salish art with influences from his mixed heritage and urban environment to create work that resonates widely across communities and cultures.
Black Sheep is about drawing power from past experiences— even traumas. It is about self-care.
“I’ve been thinking about the term baggage, and it’s all wrong. When we think about our past experiences as something we can just put down, we can’t actually heal. The real pathway to becoming stronger and more confident versions of ourselves is to learn to live in symbiosis with our past experiences.”
The Black Sheep’s body is composed of Louie’s signature wolf-mouth motif, which he uses here to symbolize negative past experiences. It is painted loosely to indicate the frequent movement of and the idea that our past experiences are living parts of us that we can’t simply set down as if they were “baggage.”
By contrast, the Black Sheep’s face is composed of highly structured Coast Salish design elements to indicate the self-confidence drawn from the understanding that past experiences make us better equipped to manage whatever lies ahead. A few understated sprouts indicate constant growth regardless of what we are experiencing.
__________________________________________________________________________________________________________________
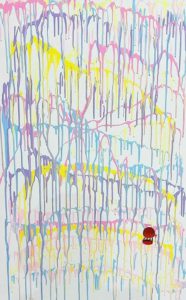
ART PIECE: Bleed Joy
ARTIST NAME: Tahira Naqvi
ARTIST INFO: I am a new artist venturing out to create artwork that speaks to mental health struggles. Childhood trauma is a big factor in my art, which is abstract and comes from the heart. It delves into deep wounds and the quest to achieve joy through self-reflection. I speak through colors and shapes that represent this journey of self-healing.
When I started on this piece, I did not know what to create, but I knew I wanted to display my pain, my joy, and my journey. So, I faced the canvas and decided to just let it flow. This piece has chaos, joy and a dark passenger. All representing the struggle between my child and adult selves. There is a hot air balloon. When I was little, I always wanted to escape. One day, I took my mom’s large shoe box and tied her red scarf to its four ends, after which, I walked out to our balcony and tried to leap off to go explore the world. Except, my grandfather saved me.
I have a natural instinct to leap forward and escape. It took cycles of anxiety to create this very personal piece. “Bleed Joy” is for everyone dealing with mental chaos and anxiety in their lives. My hope is that, by putting this out there, I will finally heal and find contentment.
_________________________________________________________________________________________________________________
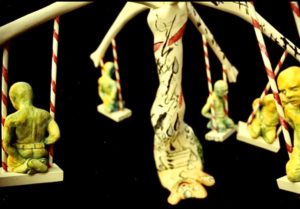
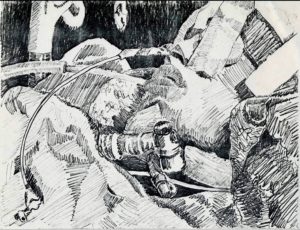
ART PIECE: Untitled
ARTIST NAME: Munira Leslie Sinclair
ARTIST INFO: Munira Leslie Sinclair was a talented visual artist, eloquent writer & devoted mother to her children, including an adult son with severe traumatic brain injury (TBI). Much of her artwork was inspired by her struggles through some very difficult times as well as the unrelenting challenges of trying to ensure quality care for her son with special needs, in a system not well set up for patients like him. A passionate patient advocate, she worked to improve the lives of those with TBI through legislation & advocacy training. While she faced adversity & bouts of cancer with fortitude, art was her outlet.
Leslie passed away on September 30, 2022. Special thanks go to her daughter, Jennifer, who has given WPSC’s Addressing Stigma & Bias Workgroup permission to share these 2 pieces with our audience.
**************************************************************************************************************************************************************************
Poetry
**************************************************************************************************************************************************************************
EVERYTHING CHANGES
Everything is touched
by the sea of time.
We are life forms
on the shore
of existence.
No matter how you try
to be immovable,
time moves you.
It caresses you,
lulls you,
embraces you.
Just as you’re buoyed
into a comfortable slumber,
it snatches you,
pulls you out
& swallows you.
It swirls you around
& sucks you in.
Then,
just as suddenly,
it floats you,
breathless,
onto its surface.
The winds of change
calm to a whisper.
You feel it
cushioning you,
as you lay
adrift
with your face to the sky.
Then it stirs,
picks you up,
carries you
on a wave;
pushes you forward,
races you
back to shore
& deposits you,
gently,
onto the sand.
Glistening in the sun,
you catch your ragged breath. And settle down.
Before long,
you’re feeling the breeze
on your face,
looking up at the stars
& thinking:
I could stay like this forever.
You inhale the stillness…
Then it wakes you
from your reverie.
It foams
at your feet,
kissing your toes,
nudging you.
It teases you
into motion.
Slowly,
you move to the tide’s rhythmic touch,
sway to its hypnotic gyrations
& join,
again,
the dance of life.
—
Tomorrow becomes today.
Today becomes yesterday. Yesterday is but a memory.
Did we remember to live in today?
© 2020 Anita Sulaiman
POEM TITLE: EVERTHING CHANGES
ARTIST NAME: Anita Sulaiman
ARTIST INFO: Anita Sulaiman is Principal Consultant and Executive Coach at IBEX Consulting, whose areas of expertise include strategy, leadership development, marketing and change management/business process re-engineering. Anita is also a culture coach specializing in cultural competency and cross-cultural communication. Helping individuals and organizations excel in a global world is a passion.
Anita stays at the forefront of efforts to improve patient safety, serving on advisory groups and committees for organizations including the Washington Patient Safety Coalition, Foundation for Health Care Quality (Patient & Family Advisory Council) and Washington State Coalition for Language Access. She is Chair of the Addressing Stigma and Bias Workgroup, a partnership between WPSC and the Bree Collaborative, a healthcare non-profit established by the Washington State Legislature.
Everything Changes was written at a time of emotional turmoil. In the midst of personal upheaval, thanks to the practice of meditation to help with her mental health, this poem about the vagaries of time captures moments of clarity from seeing that change, while invariably very stress-inducing, are part of the ebb & flow of life.
_________________________________________________________________________________________________________________
WHO AM I TRYING TO BE?
Who am I? Who am I trying to be?
Not myself, anyone but myself.
Living in a fantasy to bury the reality,
Making myself the mystery,
A strong facade disguising the misery.
Empty, but beyond the point of emptiness,
Full to brim with fake confidence,
A guard that will never be broken,
Because I broke a long time ago.
I’m hurting but don’t tell anyone.
No one needs to know.
Don’t show or you’ve failed.
Always okay, always fine, always on show.
The show must go on.
It will never stop.
The show must not go on,
But I know it will.
I give up. I give up giving up.
I am lost.
I don’t need to be saved,
I need to be found.
POEM TITLE: WHO AM I TRYING TO BE?
ARTIST NAME: Cara Delevingne
ARTIST INFO: Cara Delevingne, actress and model, shares her personal experiences with anxiety and depression.